Is Foot Pain Keeping You Up at Night?

Nighttime foot pain can disrupt sleep and make restful nights a challenge for many people. This type of discomfort frequently stems from plantar fasciitis, where the plantar fascia, the band of tissue along the bottom of the foot, becomes inflamed due to stress or overuse. Another potential cause is Morton’s neuroma, which occurs when the nerves between the toes are pinched, leading to sharp, burning sensations. Peripheral neuropathy, often linked to diabetes, may cause tingling, numbness, or stabbing pain during the night. Lifestyle factors, such as prolonged standing, wearing improper footwear, or other weight-bearing activities, can aggravate symptoms. Structural foot conditions, including flat feet or high arches, may increase susceptibility to nocturnal foot pain. A podiatrist can assess the underlying cause of nighttime foot pain and offer professional guidance on managing your symptoms. If frequent foot pain is interrupting your sleep, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. John C. Lawlor from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
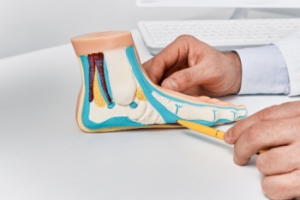
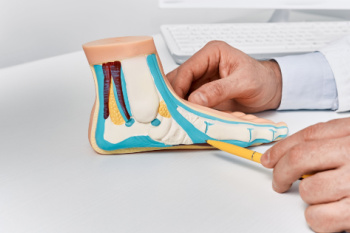
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Get Professional Care for a Broken Foot or Ankle
Facts About Heel Spurs

Heel spurs are bony growths that develop on the underside of the heel bone, typically as a result of prolonged stress or strain on the foot. The most common cause of heel spurs is plantar fasciitis, an inflammation of the tissue that connects the heel to the toes. Other factors that contribute to heel spurs include wearing improper footwear, obesity, repetitive activities that put pressure on the feet, and abnormal foot mechanics such as flat feet or high arches. While heel spurs themselves are often painless, they can lead to complications such as chronic pain, difficulty walking, and inflammation. In some cases, the spur may press on nearby nerves, causing sharp or shooting pain. If left untreated, heel spurs may limit mobility and interfere with daily activities, leading to long-term discomfort and reduced quality of life. If you have heel pain, it is suggested that you consult a podiatrist who can provide an accurate diagnosis and treatment solutions.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. John C. Lawlor from Florida. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
All About Bunions

Bunions, medically known as hallux valgus, occur when the big toe shifts toward the smaller toes, causing a bony bump to form on the inside of the foot. This misalignment often develops gradually, with genetic factors and wearng ill-fitting footwear being common contributors. The protrusion can cause discomfort, especially when tight or stiff shoes rub against it, resulting in redness, swelling, or pain around the joint. As the toe deformity progresses, it may lead to uneven pressure distribution, sometimes causing pain beneath the ball of the foot. Certain non-surgical bunion treatments, like appropriate footwear and wearing custom orthotics, can help to relieve bunion symptoms. However, surgery may become necessary when persistent pain interferes with your daily activities. A podiatrist can assess the severity of the bunion, offer specific treatments, and recommend strategies to prevent further progression. If you are suffering from bunion pain, it is suggested that you schedule an appointment with a podiatrist.
If you are suffering from bunions, contact Dr. John C. Lawlor of Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Causes and Symptoms of Adult Flat Feet
Adult flat feet occur when the arches of the feet collapse or flatten, leading to a lack of natural arch support. One common cause is excessive body weight, which places extra pressure on the feet and can weaken the arch over time. Foot or ankle injuries, such as fractures or sprains, can also damage the structures supporting the arch, leading to flat feet. Rheumatoid arthritis, or RA, is another contributor, as the inflammation it causes can affect the joints in the feet, leading to a collapse of the arch. As people age, the tendons and ligaments in the feet naturally weaken, making flat feet more common. Symptoms of adult flat feet include foot pain, swelling, and fatigue, particularly after prolonged standing or walking. If you have flat feet, it is suggested that you contact a podiatrist who can help you to manage this condition.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. John C. Lawlor from Florida. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
How to Choose the Right Running Shoes for Your Individualized Style

Choosing the right running shoes is essential to enhancing performance and preventing injury. The type of running you do plays a significant role in determining the best shoe for you. If you are a long-distance runner, look for shoes that offer plenty of cushioning to absorb impact over extended periods. For speedwork or short-distance running, lightweight shoes with a more responsive feel will help improve your pace. Trail runners require shoes with durable outsoles and better grip to handle uneven, rough terrains. Consider your foot arch and pronation as well. Those with flat feet or overpronation may benefit from shoes with added support, while high arches may need shoes with more flexibility and cushioning. Proper fit is key, so make sure there is enough room in the toe box and that the shoe feels snug without causing discomfort. If you have endured a foot injury from wearing the wrong running shoes, it is suggested that you contact a podiatrist who can treat various foot conditions, and guide you on choosing the right running shoes.
If you are a runner, wearing the right running shoe is essential. For more information, contact Dr. John C. Lawlor from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
To increase performance and avoid the risk of injury, it is important to choose the right running shoe based on your foot type. The general design of running shoes revolves around pronation, which is how the ankle rolls from outside to inside when the foot strikes the ground.
- Neutral runners are able to choose from a wide variety of shoes, including minimalist shoes or even going barefoot.
- Runners who overpronate, or experience an over-abundance of ankle rolling, should choose shoes that provide extra motion control and stability.
- Runners who underpronate, or supinate, have feet that have high arches and lack flexibility, preventing shock absorption. They require shoes with more flexibility and cushion.
If you have any questions please feel free to contact one of our our offices located in Cape Coral and LaBelle, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.